Strict Standardization of Cleaning and Disinfection Procedures for Instruments in Obstetrics and Gynaecology
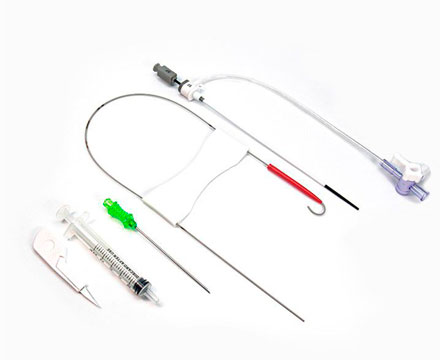
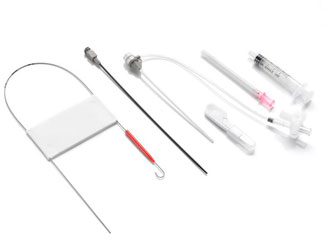
The instruments in obstetrics and gynaecology is widely used in various gynecological examinations and related treatments. With many different types and complex structures, the equipment can become contaminated with large amounts of secretions, blood, bodily fluids and other body tissues after use. It is particularly difficult to clean the uterine suction tube, and failure to disinfect and sterilize thoroughly during the cleaning process can easily lead to cross-infection. It is important to establish and improve the cleaning and disinfection process for instruments in obstetrics and gynaecology, and to strictly follow the procedures during the cleaning process.
Collection of instruments in obstetrics and gynaecology
The collection personnel should be proficient in the collection process and requirements of instruments in obstetrics and gynaecology. They should wear appropriate protective clothing, maintain good hand hygiene, avoid contaminating the surrounding environment such as elevators and departments, and reduce cross-infection in the hospital. The collection of the medical equipment should be carried out by dedicated personnel and vehicles along a designated route. If there are any specific infected instruments, they should be packaged in double-layer sealed yellow garbage bags, accurately labeled with the name of the infectious disease, and placed in a special closed box for contaminated instruments, for separate collection and disposal. The collection tools should be promptly cleaned and disinfected after use for backup.
Counting and classification of instruments in obstetrics and gynaecology
The cleaning personnel should take personal protective measures as required, and two medical staff should classify, count, verify and register the recovered equipment in the decontamination area according to the equipment list filled in by the clinical department. If there are any problems, they should communicate with the relevant department to deal with them in a timely manner.
Cleaning of instruments in obstetrics and gynaecology
The decontamination area personnel should strictly follow the cleaning procedures, and choose appropriate cleaning methods according to the characteristics of the medical equipment, such as manual cleaning, ultrasonic cleaning, and fully automatic cleaning. In order to achieve better cleaning results, the combination of manual and mechanical cleaning should be used to improve the cleaning quality.
For equipment with articulated joints, the articulations should be fully opened, and detachable parts should be removed and placed in an ultrasonic cleaning basket for cleaning. Then the vaginal speculum, suction tube and metal suction tube should be placed in a solution cleaner, cleaned with a soft brush, the threaded parts should be cleaned and then placed in a fully automatic cleaning machine for cleaning, with special attention paid to the complete opening of the vaginal speculum mouth.
For the metal suction tube cavity wall, it should be repeatedly washed with a high-pressure water gun, placed in a cleaning basket and cleaned in an ultrasonic cleaning machine for no more than 10 minutes. Then, with the appropriate soft brush according to the thickness of the tube cavity, the inner wall of the metal tube cavity should be cleaned, followed by a repeated high-pressure water gun rinse and placed in a cleaning machine for final cleaning.
Special instruments that cannot be soaked can be wiped with clean water before using a cleaning cloth dipped in cleaning solution, wiped repeatedly with pure water, and finally disinfected with 75% alcohol. For precision instruments, the cleaning guidelines provided by the manufacturer should be followed.
Packaging and sterilization standardization of instruments in obstetrics and gynaecology
According to the instruments in obstetrics and gynaecology packaging catalog, the equipment should be packaged after being checked by two people for accuracy with the package label, including the name of the item, packager's name, sterilization date, etc.
The packaging should be moderately tight and fixed with a sealing capsule. During sterilization and delivery, the package should be handled with care to ensure the integrity and sterilization quality of the medical package. During sterilization, the packaged medical equipment should be placed in a sterilization basket and sterilized with a pulse vacuum high-pressure steam sterilizer. Instruments that are not heat resistant should undergo low-temperature sterilization.
When storing, there should be gaps between the packages to facilitate steam penetration. The sterilization efficiency of each batch should be checked in batches, and a 100% sterilization success rate should be achieved to ensure sterilization effectiveness. After sterilization, the items should be stored in an aseptic storage room in the correct order, confirming that all items are within their validity period, and then following the delivery workflow for transfer to the clinical department. Proper arrangements should be made to avoid stockpiling of expired items, which should then undergo a new sterilization process.

 English
English  日本語
日本語  한국어
한국어  français
français  Deutsch
Deutsch  Español
Español  русский
русский  português
português  العربية
العربية  tiếng việt
tiếng việt  ไทย
ไทย  Malay
Malay  हिंदी
हिंदी